Serogroups
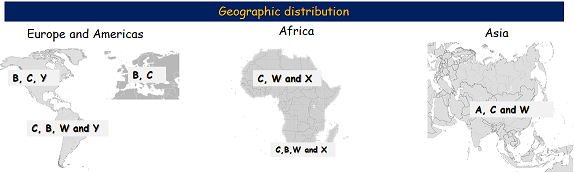
Based on capsular polysaccharides, Neisseria meningitidis can be classified into 12 serogroups, 6 of which are responsible for global epidemics, namely: A, B, C, W, X, Y. We will explore each of them with more detail. Neisseria meningitidis can also be classified in serosubtype, serotype and immunotype.
Serogroup A
Serogroup A Neisseria meningitis (MenA) was an important cause of meningitis in the African meningitis belt region before the introduction of MenAfriVac, the meningococcal group A conjugate vaccine, in 2010(1). Prior to this, attempts to halt meningitis epidemics were done using polysaccharide vaccines, with limited success(2).
During the epidemic season, disease incidence would range from 10 cases per 100 000 habitants yearly, to 1000 per 100 00 during the dry season of an epidemic year.
Since the introduction of the conjugate vaccine, no outbreak of MenA has been reported in countries where vaccination attained high coverage rates.
MenA was also the main cause of meningococcal meningitis in Europe before the 1970s, and is still is the main cause in Asia.
Serogroup B
Neisseria meningitidis serogroup B (MenB) is the main cause of menigococcal disease in Europe. Historically, the development of MenB vaccines constituted a challenge for the research community.
- The serogroup’s polysaccharide capsule contains epitopes that are very similar to that of human foetal neural tissue. They are also poorly immunogenic, with the risk of cross-reaction of antibodies.
- The alternative vaccine targets (immunogenic targets), which include sub-capsular proteins, are diverse.
Serogroup C
Neisseria meningitidis Serogroup C (MenC) caused meningitis outbreaks in US military recruits in the late 1960s (3) and was the main isolate found in parts of Europe in the 1990s, the majority due to the ST-11 clonal complex. This changed after the introduction of the conjugate vaccine in the UK in 1999. This resulted in an impressive decline in disease incidence in the UK and Europe as the vaccine was introduced in other countries.
Nevertheless, in Africa in 2017 the largest MenC outbreak was reported in Nigeria and Niger, where the vaccine had not been introduced. At this time, the MenAfriVac vaccine had already been introduced in both countries.
Serogroup W
Neisseria meningitidis serogroup W (MenW) was first reported in an army research institute in the United States in 1967. Cases due to this serogroup were uncommon until 2000, when large outbreaks started being reported. Initial cases were seen in Saudi Arabia, and then spread to South America, Europe, Africa and Australia.
A particular hallmark for these outbreaks were the atypical clinical presentation; including gastrointestinal and respiratory symptoms. Moreover, the age group most affected was different from that of other serogroups, as those commonly affected in these outbreaks were initially adults. The strains were also more virulent with case fatality rates (CFR) close to 30%. The virulent strains identified in the epidemic, were the type 11 – clonal complex (cc-11).
In Africa, an important epidemic occurred in Burkina Faso in 2002, with more than 12000 suspected cases. Moreover, in South Africa from the beginning of the 2000s, serogroup W replaced serogroup A as the most prevalent.
Serogroup X
Neisseria meningitidis serogroup X (MenX) is an uncommon cause of meningococcal disease, with few reported outbreaks. It was identified in small outbreaks in Africa in Senegal, Mali and Burkina Faso. It was previously identified in Niger in the 1990s and in 2000 and 2006, the latter with a particularly high incidence. In that year, serogroup X cases represented up to 90% of meningococcal isolates in southwestern Niger.
A conjugate MenX - TT vaccine is in development by the Serum Institute India, and preliminary results have shown that the vaccine was immunogenic in mice models.
Serogroup Y
Neisseria meningitidis serogroup Y (MenY) is mainly responsible for invasive meningococcal disease in the elderly, and a cause of pneumonia in troops in the United states. The first outbreaks of MenY in the US were reported in the 1990s.
In Europe, the incidence of MenY increased in the beginning of the 2000s and was the main cause of meningococcal disease in Sweden.
South America also observed an increase in the proportion of meningococcal disease due to serogroup Y in mid 2000s.
Currently, the tetravalent meningococcal vaccine is effective against MenY. Yet, many countries have not introduced the vaccine in their routine immunisation programmes, as the disease is still considered rare is many settings.